
As a parent, your child's well-being is always at the forefront of your mind. You celebrate their milestones, comfort them in times of distress, and ensure their overall health and happiness. Yet, amidst all these responsibilities, one crucial aspect, sometimes, could go unnoticed: your child's sleep. Recognizing pediatric sleep disorders can be challenging, as the signs are not always obvious. At Kidsville Pediatrics, we understand the silent struggles many children face when it comes to getting a good night's sleep. Sleep disorders in children can manifest in subtle ways, impacting their daily lives and overall development.
Sleep is vital for a child's physical, emotional, and cognitive growth. When sleep is disrupted, it can lead to a myriad of issues, from behavioral problems to difficulties in school. As a vigilant parent, you might notice your child is often tired, irritable, or struggling to concentrate. These could be red flags indicating an underlying sleep disorder.
Pediatric sleep disorders are more common than you might think, and they come in various forms, each with its own set of challenges. It's important to recognize the signs and seek professional guidance early on.
Common Types of Pediatric Sleep Disorders

At Kidsville Pediatrics Mansfield, recognizing and addressing sleep issues early on is crucial to avoid a cascade of negative effects. Up to 50% of children will face some sleep problems, which can lead to daytime sleepiness, irritability, and behavioral issues. For teenagers, sleep issues might even impact academic performance and increase the risk of motor vehicle crashes. Obstructive sleep apnea affects 1% to 5% of children, and diagnosing it often requires polysomnography, as it may not be apparent through a standard physical examination alone. Typically, adenotonsillectomy is the recommended treatment for this condition.
Parasomnias, such as sleepwalking and sleep terrors, are also prevalent in children. These usually occur in the first half of the night, while nightmares tend to appear later. Fortunately, only about 4% of these issues persist into adolescence, and management usually involves reassuring parents and ensuring safety rather than medical intervention.
Behavioral insomnia, a common issue characterized by difficulty falling and staying asleep, can often be managed by implementing consistent sleep hygiene practices. In some cases, extinction techniques might be necessary to help children develop better sleep patterns. For adolescents, delayed sleep phase disorder—marked by trouble falling asleep and waking up at appropriate times—can benefit from a consistent sleep-wake schedule, good sleep hygiene, and potentially, nighttime melatonin or morning bright light therapy.
Restless legs syndrome in children can be challenging to diagnose, but managing it typically involves avoiding known triggers and treating any underlying iron deficiency. Understanding these sleep patterns and disorders is crucial for parents and caregivers, and knowing when to seek professional advice from Kidsville Pediatrics Mansfield can help ensure your child gets the quality sleep they need for healthy development.
Obstructive Sleep Apnea
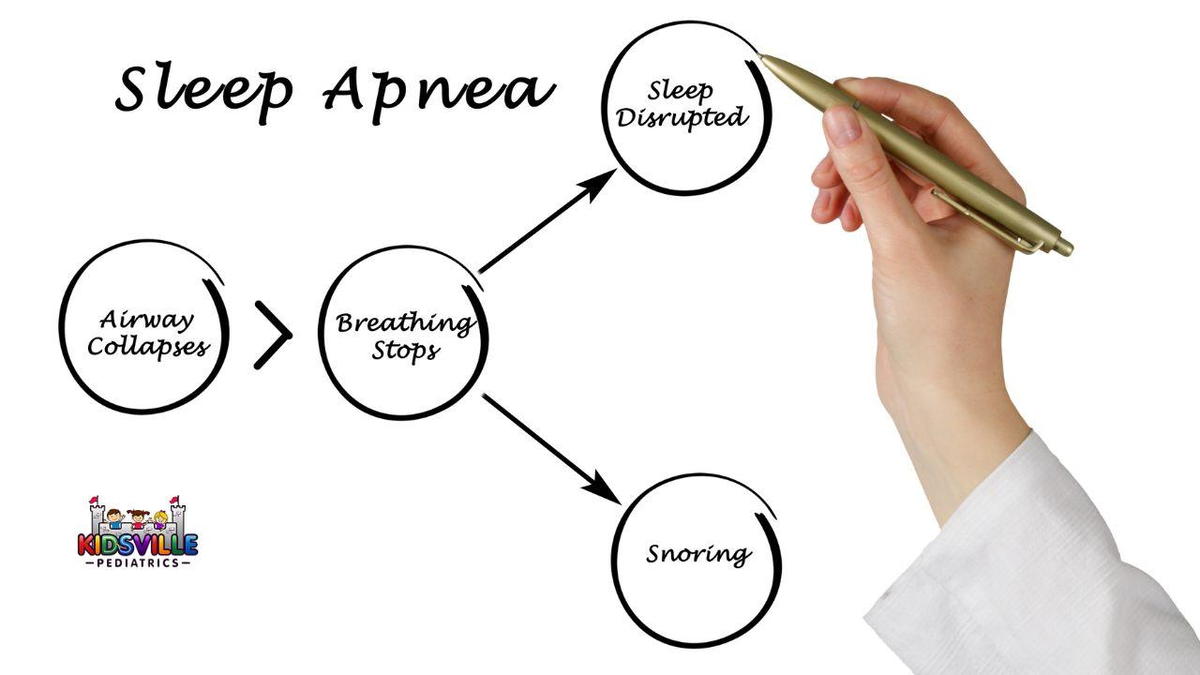
When dealing with pediatric obstructive sleep apnea, it’s crucial to understand how this sleep disorder affects your child. Unlike adults who often experience daytime sleepiness, children with sleep apnea tend to show behavioral problems. This condition arises when your child’s upper airway becomes narrowed or blocked during sleep, which can happen multiple times throughout the night.
The common causes of sleep apnea in children are larger than normal adenoids and tonsils. Adenoids are small tissue pads located at the back of the nose, while tonsils are the oval-shaped pads in the back of the mouth. Obesity, a common cause in adults, is less likely to be the issue in children. Instead, the enlarged adenoids and tonsils are usually to blame.
Symptoms of pediatric sleep apnea during the night may include snoring, pauses in breathing, restless sleep, snorting, coughing or choking, mouth breathing, nighttime sweating, bed-wetting, and sleep terrors. It’s worth noting that infants and young children might not always snore but could still experience disturbed sleep.
Throughout the day, the impact of sleep apnea on your child’s behavior can be significant. You might suddenly see that they aren’t performing well in school, or have trouble paying attention, struggling with learning, displaying behavioral problems, experiencing poor weight gain, or seemingly hyperactive.
If your child frequently wakes up feeling tired and shows persistent behavioral issues, it’s essential to consult a pediatrician. Early diagnosis and intervention are key to preventing potential complications that can affect your child's growth, cognitive development, and overall behavior. Regular check-ups with your Mansfield pediatrician can help manage and treat sleep apnea effectively, ensuring your child’s well-being and healthy development.
Somnambulance (Sleepwalking)

Sleepwalking, or somnambulance, is when a child partially wakes from sleep and walks around while still asleep. It affects about one-third of children at some point, commonly between ages four and eight, but they usually outgrow it. Despite being a concern, sleepwalking typically occurs in otherwise healthy children and is not usually linked to significant emotional or psychological issues. It generally happens during the first stages of sleep in the late evening.
If your child is sleepwalking, ensure that your home is secure and that they follow a regular sleep routine. You might notice them walking around their room or even the house, often heading towards a parent or a light source. Very young children might wander around their cot, and occasionally, they might even go outside. Although they are asleep, your child may perform simple tasks like changing clothes or moving furniture. They might also urinate in unusual places, such as cupboards or on the floor.
While sleepwalking, your child's eyes will be open but usually have a glazed look. They might engage in conversations that don’t make sense and won’t recognize you. Sometimes, they can become agitated and upset during an episode, but they won’t remember it the next morning.
Sleepwalking occurs when your child is stuck between being asleep and awake. This typically happens a few hours after falling asleep when transitioning from deep to light sleep. Illness, fever, overtiredness, or stress can exacerbate sleepwalking episodes. A family history of sleepwalking or night terrors can also play a role. Significant emotional or psychological problems are not usually the cause.
To manage sleepwalking at home, avoid waking or restraining your child. Instead, calmly redirect them back to bed after they’ve finished their activity. Keep a consistent sleep schedule, make your home safe by securing windows and doors, and remove potential hazards. Avoid making a fuss about sleepwalking, as this might upset your child and increase anxiety about bedtime. Inform caregivers if your child will be staying away overnight. If sleepwalking disrupts your family’s sleep, if your child is excessively sleepy during the day, or if you notice unusual features in their sleep patterns, it might be time to consult a doctor in Mansfield for further advice.
Somniloquy (Sleep Talking)

Sleep talking, or somniloquy, is a sleep disorder where your child talks during sleep without being aware of it. This can range from complex dialogues or monologues to simple mumbling or gibberish. It’s a common phenomenon, with up to 66% of people experiencing it at some point, though it usually happens infrequently.
Sleep talking occurs during both rapid eye movement (REM) and non-REM sleep, distinguishing it from other sleep-related vocalizations like catathrenia, which involves groaning, or REM sleep behavior disorder, where individuals act out their dreams. It is one of the more common parasomnias, with episodes often being short-lived and not necessarily linked to significant emotional or psychological issues.
Typically, sleep talking is harmless and doesn’t usually affect your child's sleep quality. The primary symptom is audible speech during sleep, which may be understandable or simply mumbling. Some studies suggest that about half of the sleep talking episodes are comprehensible, adhering to normal grammar and conversational patterns, while the rest are more disjointed or muffled.
Sleep talking may be more prevalent in children and less common in adults, though it can affect anyone. It often occurs in conjunction with other parasomnias, such as sleepwalking or teeth grinding, and can sometimes be related to dreams. If your child is sleep talking, it’s important to create a safe sleep environment and maintain a regular sleep schedule.
Although sleep talking itself is usually not dangerous, it can become problematic if it disrupts the sleep of others or leads to embarrassment. If your child's sleep talking is frequent or associated with other sleep issues, consulting a Mansfield pediatrician can help address these concerns and explore potential treatment options.
Night Terrors

Night terrors, also known as sleep terrors, can be a distressing experience for both you and your child. Unlike nightmares, which occur during REM sleep, night terrors usually happen about 2–3 hours after your child falls asleep, during non-REM sleep. During a night terror, your child might suddenly sit upright in bed, act extremely upset and scared, shout or scream, and show signs of rapid breathing and a racing heartbeat. They may also sweat, thrash around, or even get up and run from the bed. Despite the dramatic nature of these episodes, they’re typically not harmful and most children eventually grow out of them.
The underlying cause of night terrors is often related to an overexcited “fight-or-flight” response in the brain, triggered while your child is partially awake. Factors that can increase the likelihood of night terrors include not getting enough sleep, illness, certain medications, sleeping in a new place, anxiety, stress, and excessive caffeine. Additionally, conditions like obstructive sleep apnea and reflux can contribute to the frequency of night terrors.
Diagnosis usually involves a discussion of your child’s symptoms and a physical exam. Medical tests are typically not required. Treatment focuses on managing and preventing night terrors. It’s important to keep a calm demeanor and ensure your child’s safety during an episode. Try to avoid waking them as it can cause more confusion and distress. Instead, sit quietly nearby, monitor their safety, and wait for them to go back to sleep.
Preventive measures include helping your child manage stress, establishing a relaxing bedtime routine, ensuring adequate sleep, and addressing any underlying sleep disorders like obstructive sleep apnea. If night terrors occur frequently, last more than 30 minutes, or significantly affect your child’s well-being, consult a doctor in Mansfield for further guidance and possible referral to a sleep specialist.
Behavioral Insomnia of Childhood

Behavioral insomnia of childhood is a common issue affecting many families and can manifest in various ways. For young children, particularly those under two years old, sleep onset association type is prevalent. This occurs when a child struggles to fall asleep or return to sleep without specific conditions, such as having a favorite toy or a parent present. This dependency can create a demanding situation for both the child and their caregiver.
As children grow, they may develop limit-setting type insomnia, which typically begins around age two. In this case, children resist going to bed and may delay sleep with excuses like needing another bedtime story or a drink of water. Once asleep, they may refuse to return to bed if they wake up during the night. This type of insomnia becomes more common as children gain verbal skills and learn to exert their will.
Some children experience a mix of both sleep-onset association and limit-setting types, known as mixed-type insomnia. This combination can further complicate sleep routines and require tailored strategies for resolution.
The impact of insomnia on your child’s well-being can be significant. Insufficient sleep often leads to daytime difficulties, such as hyperactivity, trouble concentrating, and irritability, which can affect their performance at school and interactions with others. These issues often stem from an inability to self-soothe and develop consistent sleep habits.
Diagnosing insomnia usually involves discussing symptoms with all caregivers, as children may not clearly express their experiences. No special tests are typically needed. Treatment focuses on creating a conducive sleep environment and employing strategies such as extinction therapy. This might involve allowing the child to cry it out, implementing graduated extinction techniques, or using bedtime fading approaches to help them learn to fall asleep independently.
Delayed Sleep-Wake Phase Disorder (DSWPD)
If your child seems tired during the day but can't fall asleep until well past midnight, and then naturally sleeps in until late during vacations, they might be experiencing delayed sleep-wake phase disorder (DSWPD). This circadian rhythm disorder shifts a child's natural sleep and wake schedule later, making it difficult to align with daily obligations like school.
Children with DSWPD typically have trouble falling asleep at a desired time, often drifting off around midnight or later. Their natural wake time is delayed, making it tough for them to get up in the morning. They tend to feel most alert and functional in the late afternoon or evening. While they function well on a later schedule, conflicts with early school times or other commitments can impair their daytime performance. Untreated DSWPD can lead to social, academic, and behavioral issues, as well as depression.
This disorder is more common in adolescents and young adults, with studies showing that between 7 and 16 percent of adolescents exhibit symptoms. The causes of DSWPD are not entirely clear but may include a natural shift in sleep patterns during puberty, genetic factors, and lifestyle influences such as early school start times, late evening activities, and excessive screen time.
Diagnosis often involves a detailed history of symptoms, physical examinations, and tracking sleep patterns with logs or actigraphs. Treatment typically focuses on resetting the internal clock to align with daily demands. Options may include adjusting sleep schedules, light therapy, melatonin supplements, and improving sleep hygiene. At Kidsville Pediatrics Mansfield, a pediatrician can guide you through these steps and help manage your child’s sleep issues effectively.
Restless Leg Disorders
If you have a child with attention-deficit hyperactivity disorder (ADHD), you might notice that their difficulties with attention, impulsivity, and restlessness extend into their sleep patterns. Kids who have ADHD are more prone to sleep disorders. Two common sleep disorders associated with ADHD are restless legs syndrome (RLS) and periodic limb movements of sleep (PLMS). Studies indicate that while RLS affects about 1 in 100 children, up to 44% of children with ADHD may experience it.
Restless Legs Syndrome often manifests in children with ADHD as uncomfortable sensations in the legs, such as tingling, burning, or crawling feelings. These sensations provoke a nearly uncontrollable urge to move the legs, which can interfere with falling asleep. Many children with RLS also experience PLMS, which involves involuntary movements or jerking of the legs or arms during sleep. These movements can be frequent and disrupt sleep, leading to difficulties falling back asleep.
Periodic Leg or Limb Movements (PLMS) involve cramps and jerks that may occur from a few seconds to nearly two minutes, disrupting your child’s sleep. These movements can cause them to wake frequently, leading to poor quality sleep and affecting their mood and behavior during the day. Children with PLMS and RLS may experience increased irritability, mood swings, and difficulties in school.
The causes of these disorders aren't fully understood, but they may be linked to central nervous system issues, iron deficiencies, and certain medications. Family history can also play a role. Managing these conditions involves addressing sleep hygiene and possibly adjusting ADHD medications. At Kidsville Pediatrics Mansfield, strategies like establishing a consistent bedtime routine, ensuring a distraction-free sleep environment, and addressing any underlying nutritional deficiencies can help improve your child’s sleep and overall well-being.
Pediatrician Near Me: Visit Us at Kidsville Pediatrics Mansfield
If you’re concerned about your child’s sleep patterns or suspect they may be experiencing pediatric sleep disorders like restless legs syndrome or periodic limb movements, it's important to seek guidance from a professional. At Kidsville Pediatrics Mansfield, our team of dedicated pediatricians is here to help you navigate these challenges. We can offer tailored advice, evaluate any potential underlying issues, and develop a plan to improve your child’s sleep and overall health.
You may schedule an appointment online: https://www.kidsvillepeds.com/appointment/
Or visit/call our clinics:
Kidsville Pediatrics Mansfield TX: 682-341-3910; 1759 Broad Park Circle S, Suite 201 & 205, Mansfield, TX
Kidsville Pediatrics Southlake: 682-345-8010; 2813 W. Southlake Blvd Suite 100 Southlake, TX
Kidsville Pediatrics McKinney: 469-885-9400; 5881 Virginia Pkwy. Suite 300 Mckinney, TX
